Marvelousmellifluousvoice - Thy Hook Spares The Next Swath And All Its Twined Flowers

More Posts from Marvelousmellifluousvoice and Others

If you have Scottish and/or Irish ancestry AND red hair, you probably also have VIKING ancestry, according to a new study. The director for Nordic Studies at the University of the Highlands and Islands says red hair is modern evidence of the influence of the ancient Vikings in Celtic lands.
(via Celtic Red Hair From Vikings? - Wild Eyed Southern Celt)
Hello all you tumblr’rs out there!
Hello!
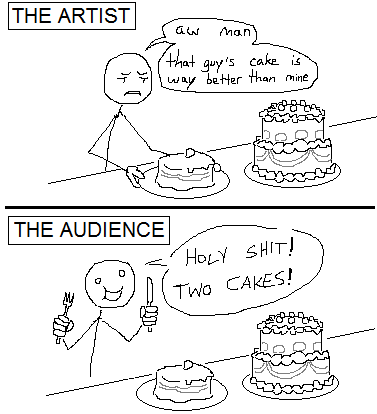
People have written a lot of touchy-feely pieces on this subject but I thought I’d get right to the heart of the matter
A doctor discovers an important question patients should be asked
This patient isn’t usually mine, but today I’m covering for my partner in our family-practice office, so he has been slipped into my schedule.
Reading his chart, I have an ominous feeling that this visit won’t be simple.
A tall, lanky man with an air of quiet dignity, he is 88. His legs are swollen, and merely talking makes him short of breath.
He suffers from both congestive heart failure and renal failure. It’s a medical Catch-22: When one condition is treated and gets better, the other condition gets worse. His past year has been an endless cycle of medication adjustments carried out by dueling specialists and punctuated by emergency-room visits and hospitalizations.
Hemodialysis would break the medical stalemate, but my patient flatly refuses it. Given his frail health, and the discomfort and inconvenience involved, I can’t blame him.
Now his cardiologist has referred him back to us, his primary-care providers. Why send him here and not to the ER? I wonder fleetingly.
With us is his daughter, who has driven from Philadelphia, an hour away. She seems dutiful but wary, awaiting the clinical wisdom of yet another doctor.
After 30 years of practice, I know that I can’t possibly solve this man’s medical conundrum.
A cardiologist and a nephrologist haven’t been able to help him, I reflect,so how can I? I’m a family doctor, not a magician. I can send him back to the ER, and they’ll admit him to the hospital. But that will just continue the cycle… .
Still, my first instinct is to do something to improve the functioning of his heart and kidneys. I start mulling over the possibilities, knowing all the while that it’s useless to try.
Then I remember a visiting palliative-care physician’s words about caring for the fragile elderly: “We forget to ask patients what they want from their care. What are their goals?”
I pause, then look this frail, dignified man in the eye.
“What are your goals for your care?” I ask. “How can I help you?”
The patient’s desire
My intuition tells me that he, like many patients in their 80s, harbors a fund of hard-won wisdom.
He won’t ask me to fix his kidneys or his heart, I think. He’ll say something noble and poignant: “I’d like to see my great-granddaughter get married next spring,” or “Help me to live long enough so that my wife and I can celebrate our 60th wedding anniversary.”
His daughter, looking tense, also faces her father and waits.
“I would like to be able to walk without falling,” he says. “Falling is horrible.”
This catches me off guard.
That’s all?
But it makes perfect sense. With challenging medical conditions commanding his caregivers’ attention, something as simple as walking is easily overlooked.
A wonderful geriatric nurse practitioner’s words come to mind: “Our goal for younger people is to help them live long and healthy lives; our goal for older patients should be to maximize their function.”
Suddenly I feel that I may be able to help, after all.
“We can order physical therapy — and there’s no need to admit you to the hospital for that,” I suggest, unsure of how this will go over.
He smiles. His daughter sighs with relief.
“He really wants to stay at home,” she says matter-of-factly.
As new as our doctor-patient relationship is, I feel emboldened to tackle the big, unspoken question looming over us.
“I know that you’ve decided against dialysis, and I can understand your decision,” I say. “And with your heart failure getting worse, your health is unlikely to improve.”
He nods.
“We have services designed to help keep you comfortable for whatever time you have left,” I venture. “And you could stay at home.”
Again, his daughter looks relieved. And he seems … well … surprisingly fine with the plan.
I call our hospice service, arranging for a nurse to visit him later today to set up physical therapy and to begin plans to help him to stay comfortable — at home.
Back home
Although I never see him again, over the next few months I sign the order forms faxed by his hospice nurses. I speak once with his granddaughter. It’s somewhat hard on his wife to have him die at home, she says, but he’s adamant that he wants to stay there.
A faxed request for sublingual morphine (used in the terminal stages of dying) prompts me to call to check up on him.
The nurse confirms that he is near death.
I feel a twinge of misgiving: Is his family happy with the process that I set in place? Does our one brief encounter qualify me to be his primary-care provider? Should I visit them all at home?
Two days later, and two months after we first met, I fill out his death certificate.
Looking back, I reflect: He didn’t go back to the hospital, he had no more falls, and he died at home, which is what he wanted. But I wonder if his wife felt the same.
Several months later, a new name appears on my patient schedule: It’s his wife.
“My family all thought I should see you,” she explains.
She, too, is in her late 80s and frail, but independent and mentally sharp. Yes, she is grieving the loss of her husband, and she’s lost some weight. No, she isn’t depressed. Her husband died peacefully at home, and it felt like the right thing for everyone.
“He liked you,” she says.She’s suffering from fatigue and anemia. About a year ago, a hematologist diagnosed her with myelodysplasia (a bone marrow failure, often terminal). But six months back, she stopped going for medical care.
I ask why.
“They were just doing more and more tests,” she says. “And I wasn’t getting any better.”
Now I know what to do. I look her in the eye and ask:
“What are your goals for your care, and how can I help you?”
-Mitch Kaminski
Source

At first I was super upset, then I read his dad’s released statement:
“Unfortunately there’s a genetic component to addiction and Indio has likely inherited it. Also, there is a lot of family support and understanding, and we’re all determined to rally behind him and help him become the man he’s capable of being. We’re grateful to the Sheriff’s department for their intervention, and believe Indio can be another recovery success story instead of a cautionary tale.”
There is strong evidence that reading for pleasure can increase empathy, improve relationships with others, reduce the symptoms of depression and the risk of dementia, and improve wellbeing throughout life, new research carried out for The Reading Agency has found.
http://readingagency.org.uk/news/media/reading-for-pleasure-builds-empathy-and-improves-wellbeing-research-from-the-reading-agency-finds.html
Read this article. Spread it around. And then point out to others that when you have your nose in a book, you are not being antisocial, and that the world would improve if they read too…
(via neil-gaiman)
Barbara Tuchman says the widespread apparently juvenile behavior of medieval Europe should be considered in light of the fact that most of active society was in fact people in their teens and twenties
Which on the one hand is like one of those things that’s obvious once it’s pointed out
But also its funny to think there was a whole historians’ tradition of being like “why were medieval kings so overemotional” until Tuchman clears her throat and goes… “Ahem… Have you ever met an eighteen year old boy” and then everyone’s like “oooooh”

Just love this one!
Another really beautiful Sam and Dean art by Lasakura. <33
-
 miratroy liked this · 4 weeks ago
miratroy liked this · 4 weeks ago -
 mehundmeh reblogged this · 1 month ago
mehundmeh reblogged this · 1 month ago -
 moavetwo reblogged this · 1 month ago
moavetwo reblogged this · 1 month ago -
 ron-ya reblogged this · 1 month ago
ron-ya reblogged this · 1 month ago -
 ron-ya liked this · 1 month ago
ron-ya liked this · 1 month ago -
 becquerelnoir reblogged this · 1 month ago
becquerelnoir reblogged this · 1 month ago -
 becquerelnoir liked this · 1 month ago
becquerelnoir liked this · 1 month ago -
 videcoeur reblogged this · 1 month ago
videcoeur reblogged this · 1 month ago -
 iswskapoiovradinavrethoumepali liked this · 2 months ago
iswskapoiovradinavrethoumepali liked this · 2 months ago -
 false798 liked this · 2 months ago
false798 liked this · 2 months ago -
 quackels reblogged this · 2 months ago
quackels reblogged this · 2 months ago -
 kawaii-little-kitty-animals reblogged this · 2 months ago
kawaii-little-kitty-animals reblogged this · 2 months ago -
 electronicdreamlandnut liked this · 2 months ago
electronicdreamlandnut liked this · 2 months ago -
 passengerhusband liked this · 3 months ago
passengerhusband liked this · 3 months ago -
 merowzers liked this · 4 months ago
merowzers liked this · 4 months ago -
 ediblenapkin-official reblogged this · 4 months ago
ediblenapkin-official reblogged this · 4 months ago -
 deatherage liked this · 4 months ago
deatherage liked this · 4 months ago -
 sadbearsreblogs reblogged this · 4 months ago
sadbearsreblogs reblogged this · 4 months ago -
 unspokenmantra reblogged this · 5 months ago
unspokenmantra reblogged this · 5 months ago -
 unspokenmantra liked this · 5 months ago
unspokenmantra liked this · 5 months ago -
 inevitable-anna liked this · 5 months ago
inevitable-anna liked this · 5 months ago -
 wacky-internet-rollercoaster reblogged this · 5 months ago
wacky-internet-rollercoaster reblogged this · 5 months ago -
 permacapslock reblogged this · 5 months ago
permacapslock reblogged this · 5 months ago -
 why-cactus reblogged this · 5 months ago
why-cactus reblogged this · 5 months ago -
 melo-cupcake-love reblogged this · 5 months ago
melo-cupcake-love reblogged this · 5 months ago -
 harmonic-psyche liked this · 6 months ago
harmonic-psyche liked this · 6 months ago -
 rebarinajar reblogged this · 6 months ago
rebarinajar reblogged this · 6 months ago -
 annal38w5 liked this · 6 months ago
annal38w5 liked this · 6 months ago -
 annita89slyzpqlkh liked this · 6 months ago
annita89slyzpqlkh liked this · 6 months ago -
 cynicalflesh liked this · 6 months ago
cynicalflesh liked this · 6 months ago -
 lemononalilypad liked this · 6 months ago
lemononalilypad liked this · 6 months ago -
 medic-simp liked this · 6 months ago
medic-simp liked this · 6 months ago -
 testsubject24601 liked this · 6 months ago
testsubject24601 liked this · 6 months ago -
 onewhoturns reblogged this · 6 months ago
onewhoturns reblogged this · 6 months ago -
 onewhoturns liked this · 6 months ago
onewhoturns liked this · 6 months ago -
 justdalek liked this · 6 months ago
justdalek liked this · 6 months ago -
 biggayarsonsbiggaytumble reblogged this · 6 months ago
biggayarsonsbiggaytumble reblogged this · 6 months ago -
 biggayarsonsbiggaytumble liked this · 6 months ago
biggayarsonsbiggaytumble liked this · 6 months ago -
 annaul82f liked this · 6 months ago
annaul82f liked this · 6 months ago -
 allthethingsiwouldnttellmom reblogged this · 7 months ago
allthethingsiwouldnttellmom reblogged this · 7 months ago -
 ironicallyahipster reblogged this · 7 months ago
ironicallyahipster reblogged this · 7 months ago -
 kaomera reblogged this · 7 months ago
kaomera reblogged this · 7 months ago
Things I like! Quotes from classic literature, nature, photography, other art- especially Vincent van Gogh, archery, and Welcome to Night Vale.
91 posts
